The novel function of PMS2 mutation on ovarian cancer proliferation
(1) Singapore American School, Singapore, (2) Department of Biological Science, University of Suwon, Wau-ri, Bongdam-eup, Hwaseong, Gyeonggi-do, Republic of Korea
https://doi.org/10.59720/22-067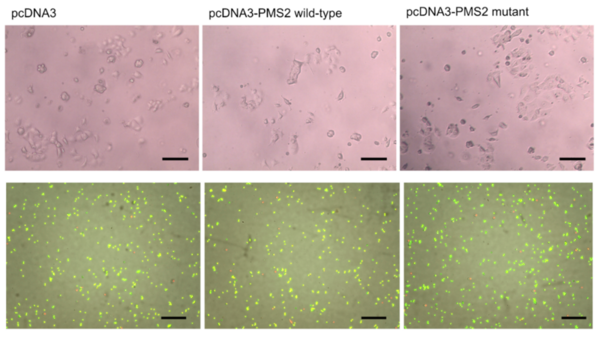
The PMS2 gene encodes a protein that plays an essential role in repairing DNA. Recent studies have shown that the S815L PMS2 mutation, rarely found in ovarian cancer (3%), causes a reduction in the PMS2 protein’s mismatch repair activity in vitro. However, no studies have focused on how this mutation affects cancer progression. Although occurrences of patients with cancers associated with the PMS2 mutation are rare, the lack of studies published on this mutation still negatively impacts their treatment. Our study aimed to discover the novel effect of this mutation in ovarian cancer cells. We hypothesized that overexpressing the wild-type PMS2 gene would have tumor-suppressive effects while overexpressing S815L PMS2 mutant would negatively affect ovarian cancer cell proliferation. We tested three transfection conditions: pcDNA3 as a negative control variant, wild-type pcDNA3-PMS2, and pcDNA3-PMS2 mutated vectors. Using RT-PCR analysis, we optimized the transfection conditions for overexpression of both the wild-type PMS2 and mutant genes in OVCAR-3 cells. We acquired microscopic images to observe cell morphology and colonization. Also, we performed a Prestoblue assay to quantify the number of live cells in each condition. Results showed that the pcDNA3- PMS2 mutated vector has a higher cell proliferation than the wild-type vectors. As hypothesized, overexpressing the wild-type PMS2 gene had tumor-suppressive effects. This observation shows that the pcDNA3-PMS2 mutation has a tumor-progressive impact on the OVCAR-3 cells. Overall, we conclude that the PMS2 mutation has tumor-progressive effects in ovarian cancer cells while the unmutated version of the gene does not.
This article has been tagged with: