C reactive protein and risk of neurological deficits and disability in patients with acute ischemic stroke
(1) Dupont Manual High School, (2) Department of Neurology, University of Louisville, (3) Department of Pediatrics, University of Louisville
https://doi.org/10.59720/24-053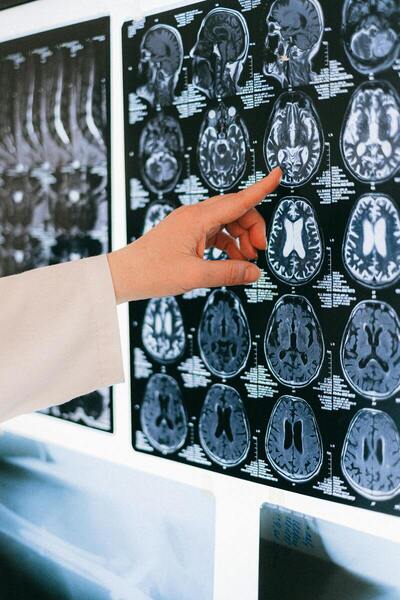
Stroke is associated with significant clinical morbidity and mortality. Previous studies have speculated on the role of inflammation in acute ischemic stroke and cardiovascular disorders. Here, we retrospectively assessed the relationship between high sensitivity C reactive protein (hsCRP) levels at stroke onset and neurological and functional morbidity, using different scales like the Barthel Index (BI) for activities of daily living, National Institutes of Health Stroke Scale (NIHSS) for stroke severity, and modified Rankin Scale (mRS) for neurologic disability. We hypothesized that higher hsCRP levels would be significantly associated with the severity of acute ischemic stroke reflected in terms of the above scales. We performed univariate analysis on data from 576 subjects and found that participants with serum hsCRP concentration > 3 mg/L exhibited higher NIHSS score, higher mRS, and lower BI. We also found that subjects with higher hsCRP had significantly increased duration of hospital stay. Logistic binomial regression did not detect statistically increased odds of more severe stroke with higher hsCRP levels. However, our model did suggest increased odds of higher disability with prior history of stroke and in males. In conclusion, higher hsCRP levels in the context of acute ischemic stroke were exhibited in subjects with significant neurological deficits (higher NIHSS scores) and greater disability at onset of stroke (higher mRS scores and BIs). However, these findings did not appear to be causal or increase the odds ratio in our multiple logistic regression model.
This article has been tagged with: