Application of gene therapy for reversing T-cell dysfunction in cancer
(1) Yongsan International School of Seoul, 285 Itaewon-ro, Yongsan-gu, Seoul, Republic of Korea, (2) Department of Biological Science, University of Suwon, Wau-ri, Bongdam-eup, Hwaseong, Gyeonggi-do, 16419, Republic of Korea
https://doi.org/10.59720/22-024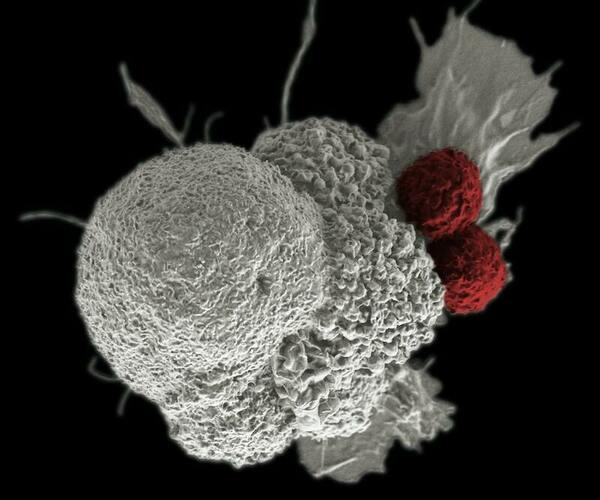
T cells are the key players of antitumor function that sense antigens produced by tumor cells and specifically target cancer cells to induce cell death. Therefore, it is widely understood that T cells are critical for cancer immunotherapy. Many recent studies discovered that T cells enter a dysfunctional or inactivated state. Cancer cells induce functional impairment of T cells by sustained expression of inhibitory receptors in T cells. Therefore, reversing T-cell dysfunction is critical for increasing the efficacy of tumor immunotherapy. In this research, we analyzed the cellular inhibition and activation of T cells using two cell line models: Jurkat (T cells) and MDA-MB-231 (breast cancer cells). We hypothesized that the knockdown of T-cell inhibition-causing genes might reverse the T-cell dysfunction caused by cancer cells. Therefore, we targeted Proprotein Convertase Subtilisin/Kexin Type 1 (PCSK1) gene in T cells and programmed death-ligand 1 (CD274) in cancer cells. We used small interference RNA (siRNA) to knock down the target gene. We used four μg/ml of lipopolysaccharide (LPS) to activate Jurkat cells. MDA-MB-231 co-culture with Jurkat cells reduced IL-2 expression level on Jurkat cells. We found that siRNA targeting CD274 in MDA-MB-231 reversed the reduced IL-2 expression level on Jurkat induced by Jurkat and MDA-MB-231 co-culture. Also, when the PCSK1 knockdown Jurkat cells and CD274 knockdown MDA-MB-231 were co-cultured, the most effective recovery of IL-2 expression level in Jurkat cells was observed. Overall, this study provides a novel strategy for reactivating T cells whose activation has been suppressed from cancer cells.
This article has been tagged with: